By Dr. Chettasak Tulayaphanich – Gender-Affirming Surgery Specialist at WIH International Hospital, Bangkok
Overview
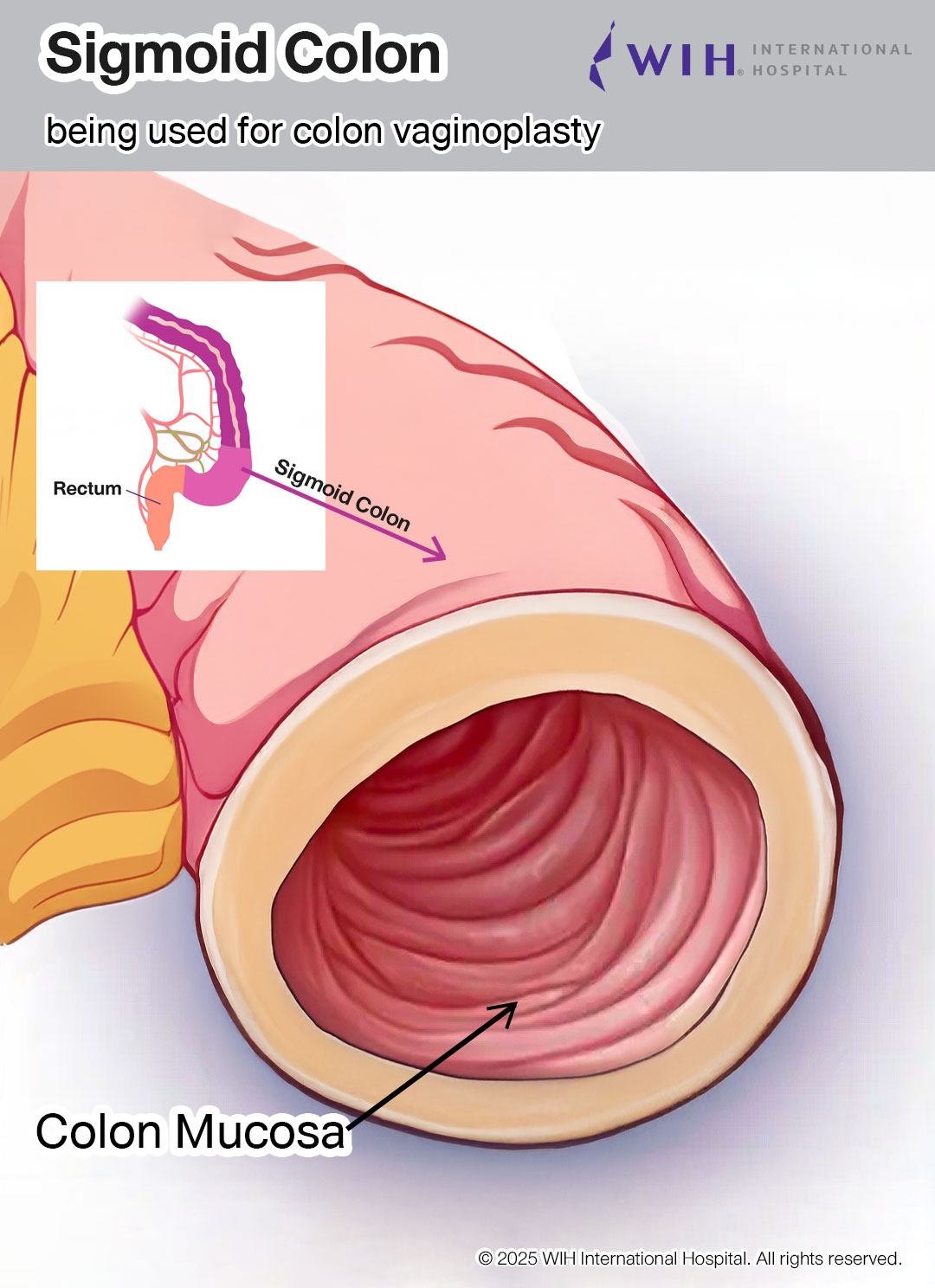
Colon vaginoplasty is an advanced surgical technique that creates a vagina using a section of the colon. Dr. Chettasak Tulayaphanich has been successfully performing this method for more than 20 years at WIH International Hospital, offering unique advantages, particularly the natural ability to produce lubrication.
Key Benefits of Colon Vaginoplasty
1. Natural Lubrication
The colon lining naturally produces mucus, which keeps the vagina moist at all times. This eliminates the need for external lubricants during intimacy, providing a significant advantage over other surgical techniques.
2. Soft and Durable Texture
The soft and thick texture of the colon lining creates a natural feel during sexual activity. The vagina becomes more flexible, which means that even if your partner is on the larger side, there’s usually no injury or tearing. This durability makes it a superior option for long-term function.
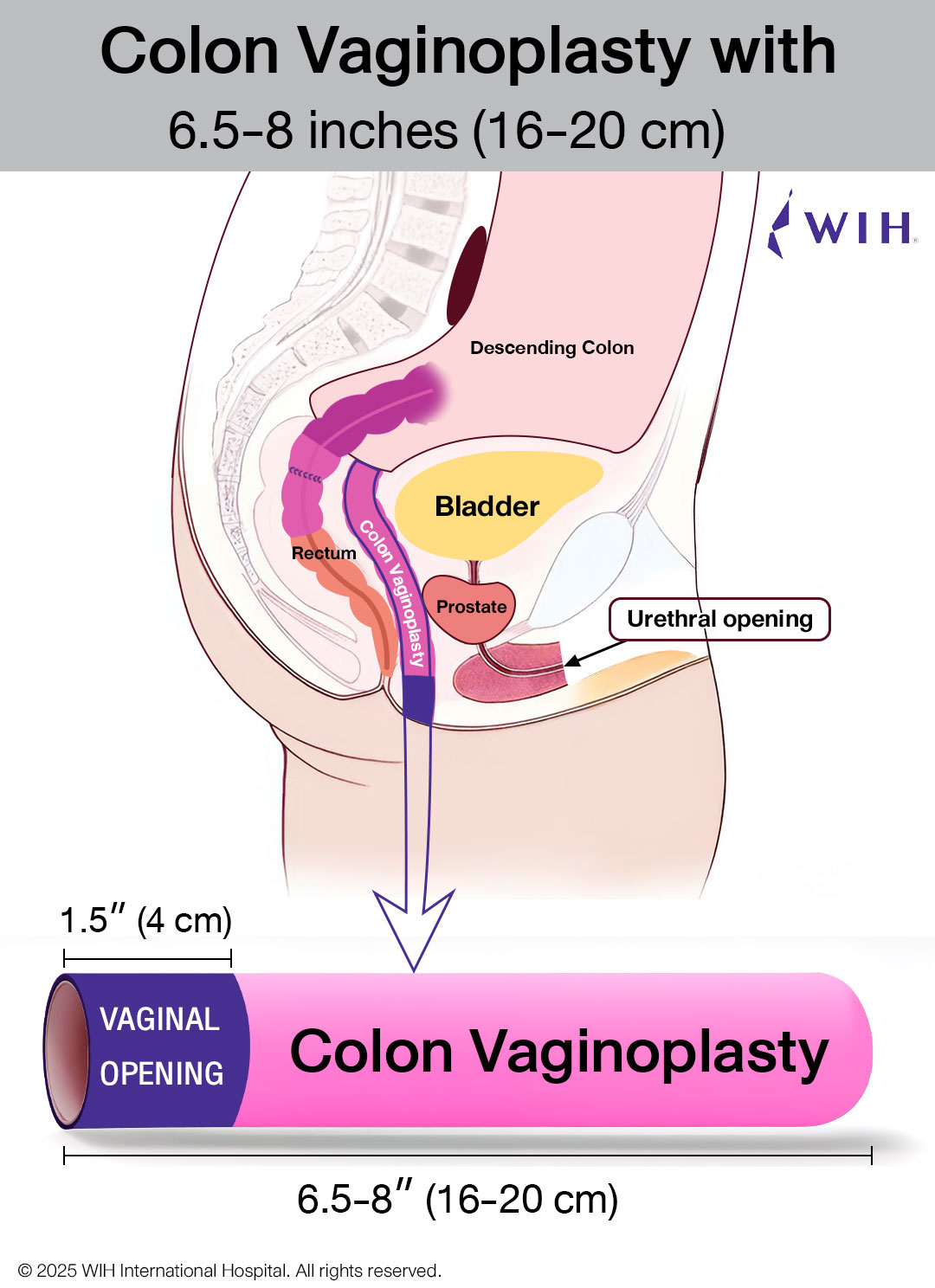
3. Optimal Depth
You can expect at least 7 inches of usable depth with this technique. The sigmoid colon typically provides around 7-8 inches of length, which is sufficient to reach the vaginal opening after proper positioning during surgery.
4. Naturally Hairless
The colon lining is naturally hairless, eliminating concerns about whether hair removal was performed properly, which is a common issue with skin graft techniques.
Important Considerations of Colon Vaginoplasty
Moisture Management
While the natural lubrication is generally beneficial, some patients might feel “too wet” in daily life, especially in the early stages before the body balances things out. The amount of mucus can vary from person to person during the initial healing period.
Odor Concerns
Many patients worry about potential odors, but colon vaginoplasty doesn’t produce any unpleasant smells. The section of colon used is completely separated from the digestive system, so it doesn’t carry any waste or bacteria. If you maintain good health and normal hygiene, the result will be fresh and natural, just like a biological vagina.
Cost Considerations
Colon vaginoplasty is more expensive than skin graft vaginoplasty because it’s a more complex surgery. The procedure involves operating inside the abdomen to prepare and reattach the colon, requiring specialized expertise. However, for patients seeking the unique features of natural lubrication, soft durable lining, and freedom from hair concerns, colon vaginoplasty is absolutely worth the investment.
Surgical Procedure: Dr. Chettasak’s NPI Technique with Colon Vaginoplasty
Dr. Chettasak Tulayaphanich performs this advanced procedure combining his signature NPI (Non-Penile Inversion) technique with colon vaginoplasty to provide optimal aesthetic, sensory, and functional outcomes at WIH International Hospital.
External Genital Reconstruction Using Dr. Chettasak’s NPI Technique
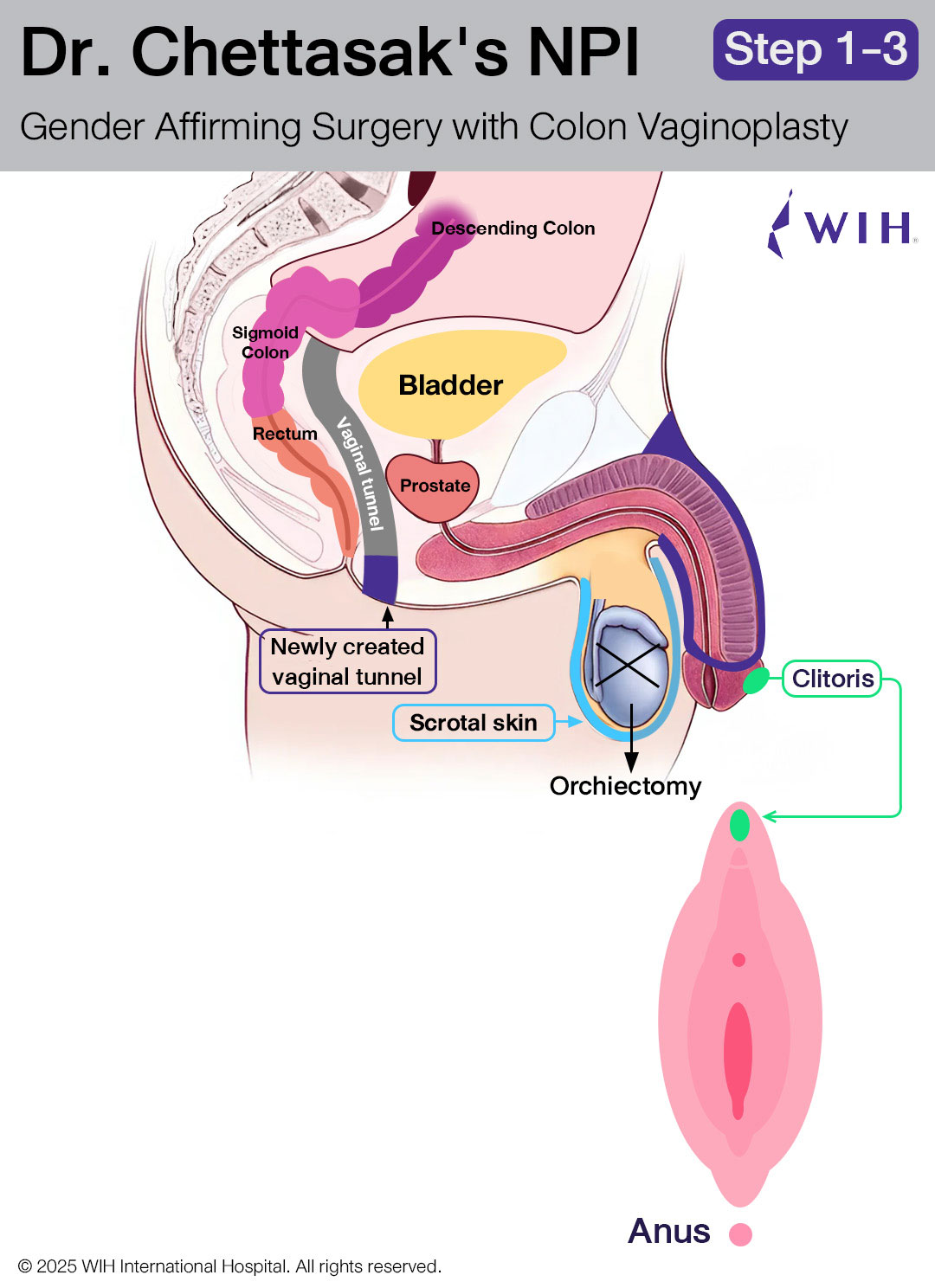
Step 1: Designing the Vaginal Opening and Creating the Tunnel
Dr. Chettasak begins by designing the vaginal opening, with careful incorporation of the perineal skin to form the floor of the new vaginal entrance. This approach enhances the natural appearance and structure of the vaginal introitus.
Next, a tunnel is meticulously created to follow the anatomical pathway of a natal female. This tunnel runs just beneath the urethra and behind the bladder, extending toward the posterior pelvic cavity, where it will later be connected to the abdominal cavity. This prepared space will receive the sigmoid colon segment during the next surgical phase.
Step 2: Bilateral Orchidectomies
Both testicles are surgically removed in a procedure known as bilateral orchidectomy. During this step, the entire spermatic cord is also carefully excised, with the cut made as close as possible to the external ring of the inguinal canal. This technique helps create a smoother contour in the groin area and reduces the risk of palpable remnants.
Importantly, the scrotal skin is preserved in optimal condition, as it will be used in the later stages to construct the outer labia (labia majora), ensuring a natural and feminine aesthetic outcome.
Step 3 : Clitoris and Clitoral Hood Reconstruction
The clitoris is reconstructed from the dorsal part of the glans penis, using a precise dissection technique to maintain maximum sensory function. Dr. Chettasak meticulously preserves the clitoral neurovascular pedicle, ensuring the branches of the pudendal nerve remain intact to support long-term erogenous sensation.
To provide an aesthetically natural appearance, the clitoral hood is created using a portion of the prepuce skin, mimicking the protective fold of tissue found in natal female anatomy. This step not only enhances the appearance but also helps reduce direct friction on the clitoris, contributing to postoperative comfort and sexual function.
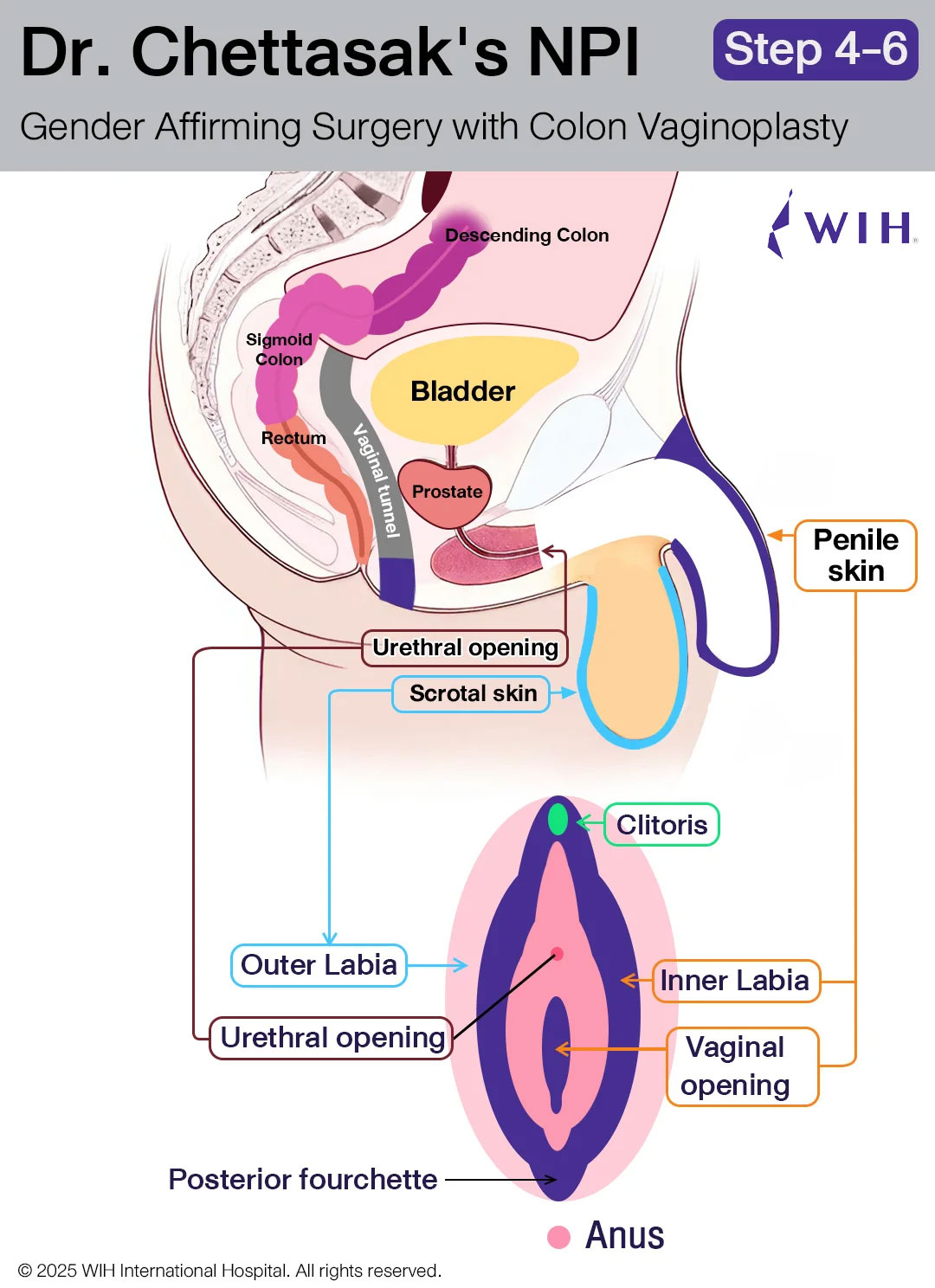
Step 4: Penectomy and Urethral Reconstruction with Penile Skin Preservation
The penis is removed through a careful penectomy, during which the entire corpus spongiosum—the spongy tissue surrounding the urethra—is also completely excised to prevent residual erectile tissue and improve surgical precision.
At the same time, the urethra is shortened and repositioned to align with typical female anatomy. A new urethral opening is reconstructed just above the introitus (vaginal entrance) to mimic the natural female location.
Throughout this step, Dr. Chettasak Tulayaphanich ensures that the penile and prepuce skin are preserved in optimal condition. These tissues will be used in the following step to create the inner labia and a natural-looking vaginal opening as part of Dr. Chettasak’s signature NPI technique.
Step 5: Inner Labia, Vaginal Opening, and Posterior Fourchette Reconstruction
Using the preserved penile and prepuce skin, Dr. Chettasak Tulayaphanich carefully reconstructs the inner labia and sculpts a natural-looking vaginal opening with a delicate V-contour. This approach ensures a feminine and realistic appearance.
A key part of this step is the precise creation of the posterior fourchette—the natural joining point at the lower end of the vaginal opening—using the inner folds of preserved skin. This detail enhances both the aesthetic and anatomical authenticity of the vagina.
This reconstruction method is the signature feature of Dr. Chettasak’s Non-Penile Inversion (NPI) technique, which is globally recognized for delivering superior cosmetic and sensory outcomes in gender-affirming surgery.
Step 6: Outer Labia Reconstruction
The outer labia are reconstructed using the preserved scrotal skin, completing the external genital reconstruction phase.
Colon Harvesting and Integration Phase
Step 7: Colon Segment Selection and Preparation
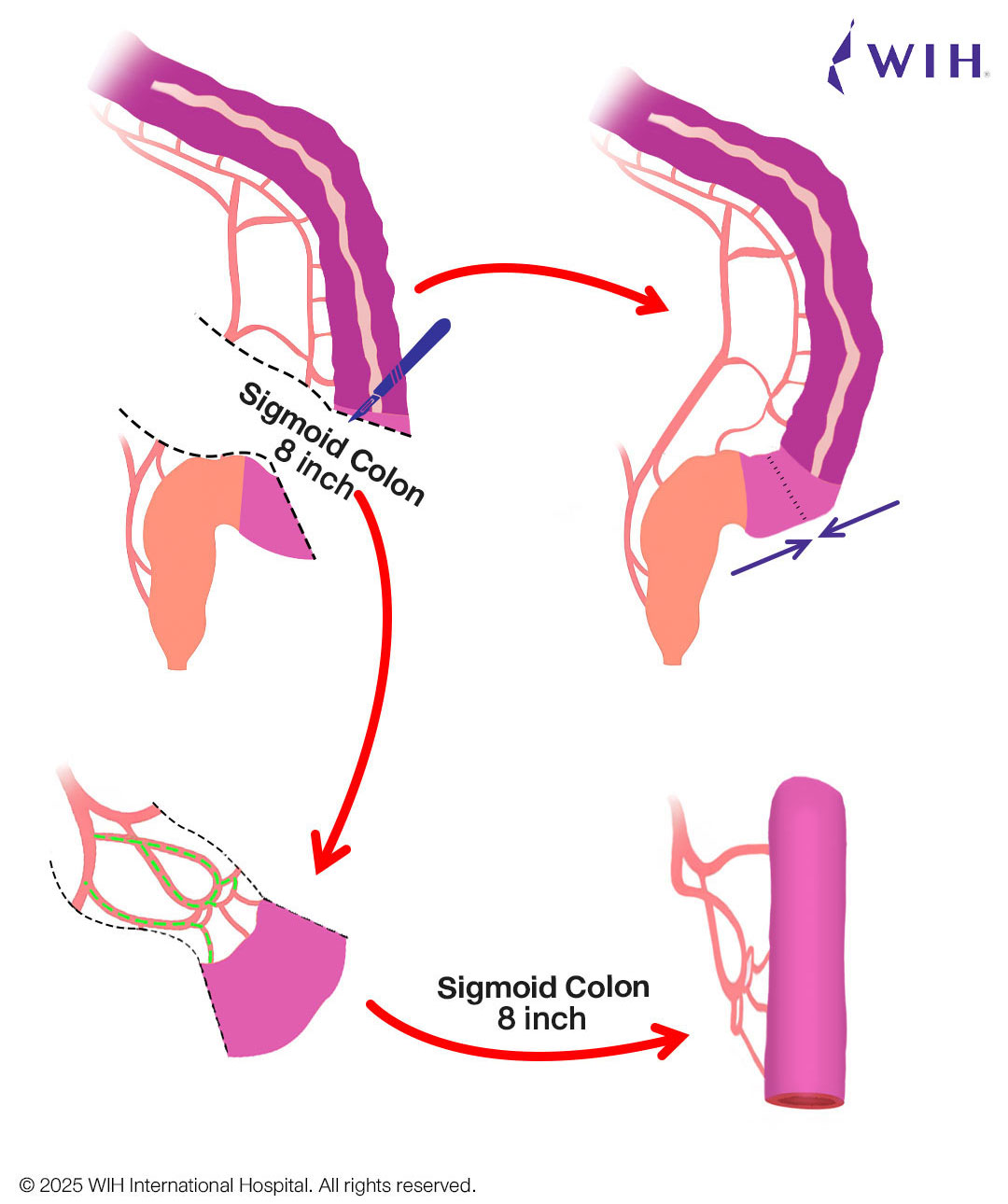
Dr. Chettasak’s colorectal surgery partner performs this phase through minimally invasive laparoscopic surgery. An 8-inch segment of sigmoid colon is selected and fully separated from the original digestive tract. Both ends are cut, but the blood supply is carefully preserved. The colon segment is then rotated and moved down to the pelvic area, ready for placement into the vaginal tunnel.
Step 8: Digestive Tract Restoration
The remaining colon is securely reconnected to ensure that digestive function remains completely normal after the procedure.
Step 9: Creating the Vaginal Vault
One end of the harvested colon segment is carefully closed to form the deepest portion of the neovagina, also known as the vaginal vault. This closure helps define the internal endpoint of the vaginal canal and ensures a smooth, rounded base that mimics natural female anatomy.
The prepared colon segment is now ready to be positioned into the vaginal tunnel in the next step.
Step 10: Securing the Colon Segment at the Vaginal Opening
To complete the vaginal formation, the open end of the colon is carefully secured to the vaginal opening. Prior to this, a surgical window is created near the cul-de-sac area to connect the vaginal tunnel (created in Step 1) with the abdominal cavity, allowing smooth passage of the colon segment into its final position.
Once the colon segment is guided through this tunnel, the open end is meticulously sutured to the deep portion of the vaginal introitus. This precise integration ensures that the colon lining is not visible from the outside, maintaining a natural aesthetic while providing a fully functional neovagina with self-lubricating capability.
Step 11: Secure the Colon Flap in Place
Once the new vaginal lining is in position, Dr. Chettasak’s colorectal surgery partner also fixes the upper part of the colon flap to the side of the abdominal wall. This helps keep it stable and prevents the colon from sliding or moving downward into the vaginal canal — which could cause a bulge or prolapse later on.
Step 12: Initial Healing Support
Gauze packing is placed inside the new vaginal canal for 5 days to keep the canal expanded during the critical early healing period.
Top 3 Benefits of Dr. Chettasak’s NPI Technique with Laparoscopic Colon Vaginoplasty
Benefit 1: Exceptional Sensation & Natural-Looking Genital Appearance
Dr. Chettasak’s signature NPI (Natural Posterior Integration) technique preserves the sensory nerves from the glans penis to create a fully sensate clitoris. The labia minora and vaginal opening are sculpted with artistic precision to mimic natural female anatomy, giving patients both beauty and function.
Benefit 2: Entire Vaginal Canal Made from Colon — No Penile Inversion
Unlike traditional vaginoplasty techniques, Dr. Chettasak completely avoids penile inversion. Instead, he uses a segment of the colon to construct the entire vaginal canal. This approach eliminates the risk of hair growth inside the neovagina, while providing excellent depth, natural self-lubrication, soft texture, and long-term durability.
This colon-based method — exclusively performed with laparoscopic harvesting — results in a functional and comfortable vaginal canal that mimics natal anatomy far more effectively than skin graft alternatives.
Laparoscopic colon vaginoplasty offers significant advantages over the traditional open technique — including smaller scars, less pain, faster recovery, and a lower risk of bowel adhesions or obstruction, especially in patients with high BMI. For more details, please see: Benefits of Laparoscopic Technique for Colon Vaginoplasty Compared with Traditional Open Technique.
Benefit 3: Natural External Appearance with Hidden Colon Tissue
While the inside of the vagina is lined with colon tissue, Dr. Chettasak ensures that it remains entirely hidden. The external vulva is formed using pink mucosal tissue and custom skin grafts, creating a natural-looking appearance without any visible signs of colon lining.
Why Choose Dr. Chettasak’s Colon Vaginoplasty with NPI Technique?
This advanced gender-affirming surgery offers unparalleled functional and aesthetic results — including natural lubrication, optimal vaginal depth, and a hair-free canal. While the procedure is more complex and involves higher costs than traditional methods, patients consistently report that the superior outcome and Dr. Chettasak’s expertise make it a life-changing and worthwhile investment.
Colon Vaginoplasty: The Gold Standard for Treating Vaginal Narrowing and Stenosis in Revision Surgery
Colon vaginoplasty is widely recognized as the most effective revision technique for transgender women facing complications after their initial gender-affirming surgery — including vaginal narrowing, stenosis, or insufficient depth.
Before reconstructing the vaginal canal, all remaining skin from the original neovagina must be carefully removed to prevent future complications.
At WIH International Hospital in Bangkok, Dr. Chettasak Tulayaphanich and his expert surgical team specialize in advanced laparoscopic colon vaginoplasty. This minimally invasive approach offers enhanced precision, reduced scarring, and faster recovery — ensuring both functional and aesthetic success in complex revision cases.
Why Colon Tissue Is the Best Choice for Revision Vaginoplasty
1. Dedicated Blood Supply for Better Healing
Colon tissue has its own blood supply, which allows it to thrive even in areas with heavy scarring or poor tissue quality. This is particularly important in revision surgery, where previous procedures may have compromised local tissue.
2. Durable and Resistant to Shrinkage
Unlike skin grafts, colon tissue is thick, durable, and highly resistant to friction. This makes it less prone to contraction or stenosis, helping to maintain the vaginal canal’s width and function long-term.
3. Natural Lubrication
The colon naturally produces mucus, offering consistent self-lubrication. This feature improves comfort during intercourse and significantly reduces the need for artificial lubricants.
4. Provides Adequate and Lasting Depth
Colon vaginoplasty consistently achieves a vaginal canal depth of 6 to 7 inches. This makes it ideal for patients who previously experienced depth loss or non-functional neovaginas due to scarring.
Explore More:
– Secondary Colon Vaginoplasty for Treating Vaginal Narrowing or Stenosis
Colon Vaginoplasty: The Gold Standard for Treating Recto-Vaginal Fistula
Recto-vaginal fistula is a rare but serious complication after gender-affirming surgery, causing stool to leak into the neovagina. When direct repair fails due to scarring and tissue weakness, colon vaginoplasty becomes the most reliable solution, offering durable reconstruction, better depth, and natural lubrication.
Explore More:
-Secondary Colon Vaginoplasty for Treating Recto-Vaginal fistula
-Secondary Colon Vaginoplasty for Treatment for Women with Vaginal Agenesis (Absent or Underdeveloped Vagina)
Conclusion
Dr. Chettasak’s colon vaginoplasty with Non-Penile Inversion technique represents a significant advancement in gender-affirming surgery, offering unique benefits that make it an excellent choice for many patients. The combination of natural lubrication, optimal depth, soft texture, and hairless lining provides both functional and aesthetic advantages that can greatly enhance quality of life.
While the procedure is more complex and costly than traditional skin graft techniques, the long-term benefits and Dr. Chettasak’s proven expertise often justify the investment for patients seeking the most natural and functional results possible.