Treatment for Women with Vaginal Agenesis (Absent or Underdeveloped Vagina)
What is Vaginal Agenesis?
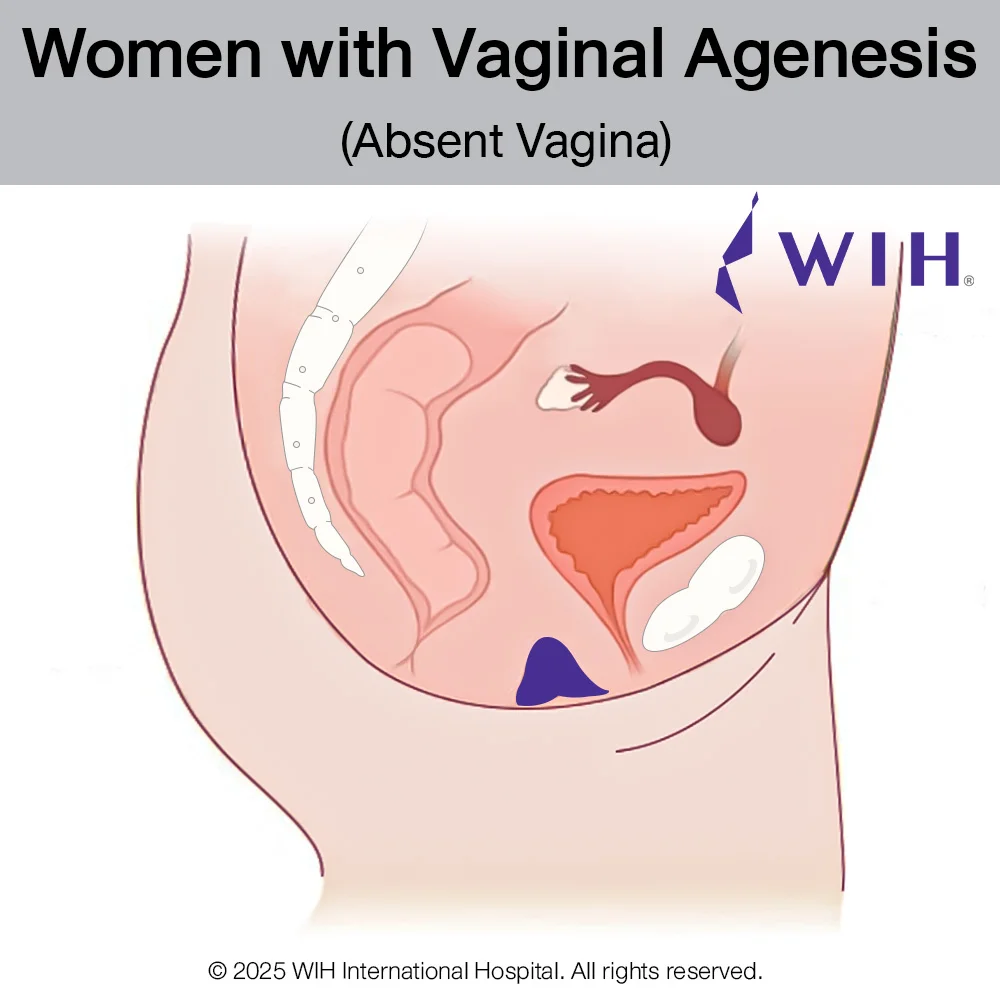
Vaginal agenesis is a rare congenital condition where the vaginal canal fails to develop properly. This condition may occur alone or as part of Müllerian agenesis, also known as MRKH syndrome (Mayer-Rokitansky-Küster-Hauser). Affected individuals are typically genetically female (46,XX) with normal external genitalia and functioning ovaries, but they lack a fully formed vagina and uterus.
Vaginal agenesis is a rare congenital condition in which the vaginal canal fails to develop completely or is entirely absent. This condition may occur on its own or as part of Müllerian agenesis, also known as MRKH syndrome (Mayer-Rokitansky-Küster-Hauser).
Affected individuals are typically genetically female (46,XX) with normal external genitalia and functioning ovaries, but they have no functional vaginal canal — in many cases, only a small vaginal dimple or shallow pouch is present at the vaginal opening. The uterus is also absent or underdeveloped.
This variation in vaginal length is crucial when selecting treatment:
- If a shallow vaginal remnant is present with a depth of at least 3 inches (approximately 7–8 centimeters), non-surgical dilation therapy may be a suitable option for creating a functional vaginal canal.
- If the vagina is completely absent or dilation fails, surgical vaginoplasty is the preferred option.
How is Vaginal Agenesis Diagnosed?
Vaginal agenesis is typically diagnosed during adolescence, when a young woman presents with primary amenorrhea (no menstrual periods) despite having normal breast development and pubic hair, which indicate functioning ovaries. Some may also report difficulty with vaginal penetration or using tampons.
Diagnosis involves a per vaginal examination to assess the presence and depth of the vaginal canal. Imaging studies such as ultrasound or MRI are used to evaluate the development of the uterus and upper vaginal structures. In addition, karyotyping is performed to confirm a normal female chromosomal pattern (46,XX).
🔍 Why Choose Colon Vaginoplasty?
If the vagina is completely absent or if dilation fails, secondary colon vaginoplasty is considered the most effective and reliable solution.
Compared to other options:
- Skin graft vaginoplasty often requires harvesting skin from distant sites like the abdomen, which can result in morbid donor site scars and dry, non-lubricating vaginal lining.
- Peritoneal vaginoplasty (PPV) is generally less reliable when used to line the entire vaginal canal. It carries higher risks of incomplete or poor healing, particularly at the distal part near the vaginal opening, where blood supply is more limited. There’s also a higher risk of vaginal contraction or stenosis, especially in patients who are unable to engage in a routine vaginal dilation program after surgery. This makes PPV a less ideal option for individuals with complete vaginal agenesis or those seeking a low-maintenance, long-term solution.
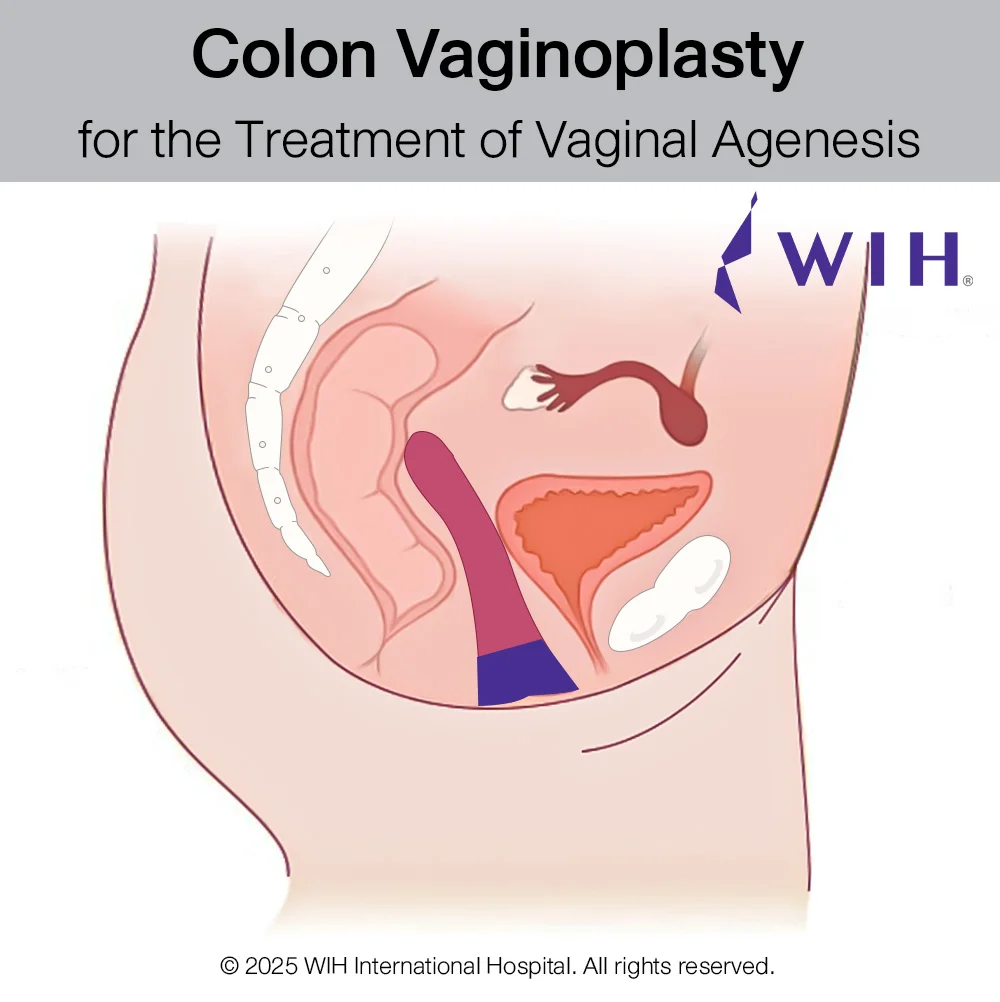
At WIH Hospital, this procedure is performed using a laparoscopic approach, which offers the benefits of smaller incisions, faster recovery, and more precise anatomical reconstruction.
