Peritoneal Vaginoplasty, also called the Peritoneal Pull‑Through Vaginoplasty (PPV), uses the thin, smooth peritoneal lining of the abdominal cavity to create the neovaginal canal. This laparoscopic, minimally invasive approach forms a moist, naturally contoured vaginal canal that resembles cis-female anatomy.
Peritoneal Pull-Through Vaginoplasty (PPV)
Benefits of PPV
• Moist, glistening lining with a smooth, natural texture
• Elastic and durable, promoting long‑term neovaginal integrity
• Minimal scarring due to laparoscopic access
• Optimal depth: ~6–7 inches (15–17 cm), sufficient for functional needs
When PPV Is Recommended
Ideal for patients who:
• Want a naturally moist canal without external grafts
• Lack sufficient genital tissue for skin‑graft methods
• Prefer a durable, low‑maintenance option without risk of deep graft shrinkage
• Seek laparoscopic surgery for quicker recovery and minimal scars
Step-by-Step Procedure
1. Laparoscopic access & peritoneum preparation
Small abdominal incisions are made to harvest a carefully preserved peritoneal flap .
2. Canal creation & peritoneum pull-through
A vaginal tunnel is formed, and the peritoneal flap is drawn into place and anchored to line the canal .
3. Refinement & closure
External genitalia are reshaped, and the new canal is tailored for both function and appearance.
Surgical Procedure: Dr. Chettasak’s NPI Technique with Peritoneal Vaginoplasty
Dr. Chettasak Tulayaphanich performs this advanced procedure combining his signature NPI (Non-Penile Inversion) technique with Peritoneal Vaginoplasty to provide optimal aesthetic, sensory, and functional outcomes at WIH International Hospital.
External Genital Reconstruction Using Dr. Chettasak’s NPI Technique
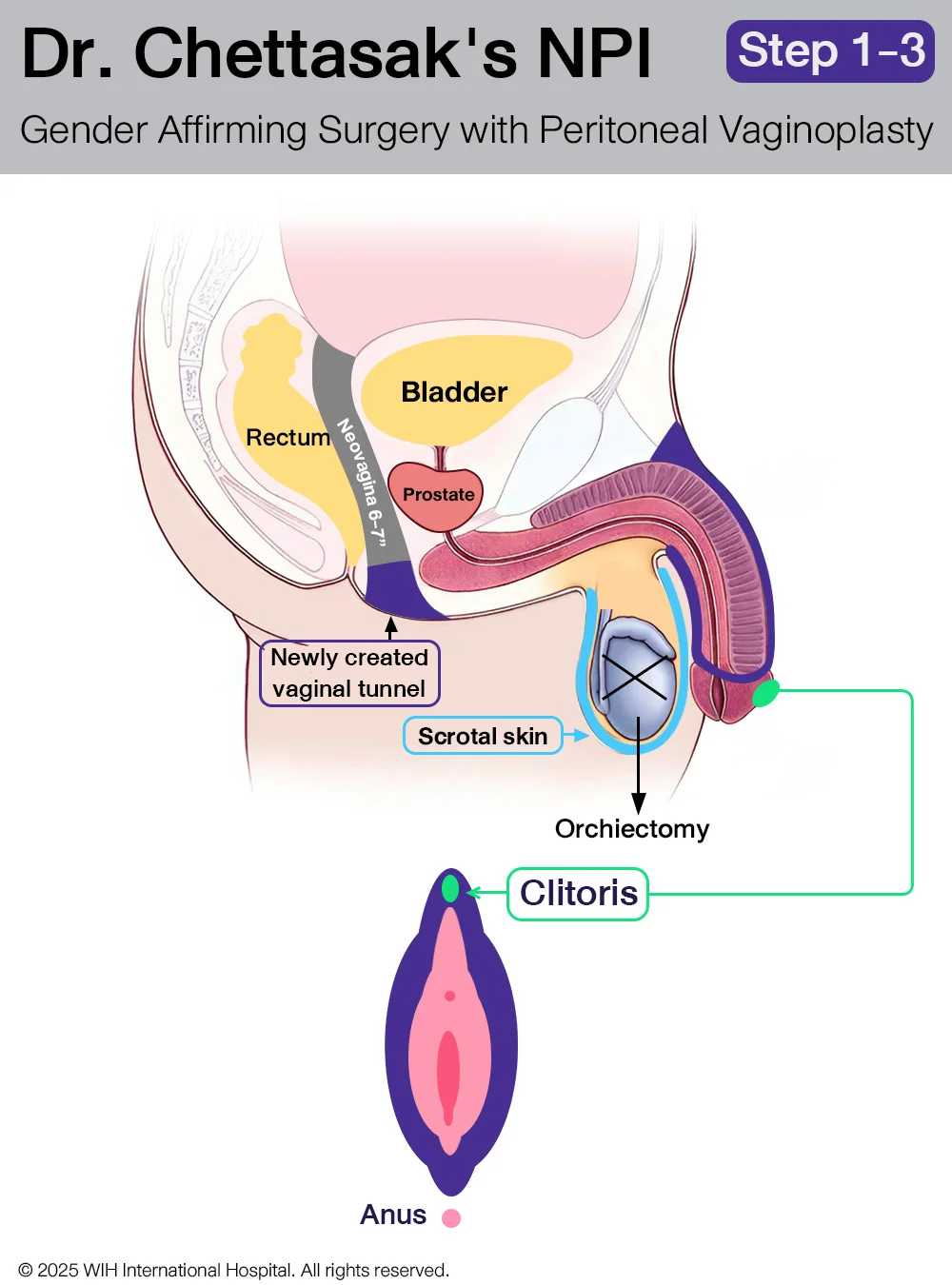
Step 1: Designing the Vaginal Opening and Creating the Tunnel
Dr. Chettasak begins by designing the vaginal opening, with careful incorporation of the perineal skin to form the floor of the new vaginal entrance. This approach enhances the natural appearance and structure of the vaginal introitus.
Next, a tunnel is meticulously created to follow the anatomical pathway of a natal female. This tunnel runs just beneath the urethra and behind the bladder, extending toward the posterior pelvic cavity, where it will later be connected to the abdominal cavity. This prepared space will receive the sigmoid colon segment during the next surgical phase.
Step 2: Bilateral Orchidectomies
Both testicles are surgically removed in a procedure known as bilateral orchidectomy. During this step, the entire spermatic cord is also carefully excised, with the cut made as close as possible to the external ring of the inguinal canal. This technique helps create a smoother contour in the groin area and reduces the risk of palpable remnants.
Importantly, the scrotal skin is preserved in optimal condition, as it will be used in the later stages to construct the outer labia (labia majora), ensuring a natural and feminine aesthetic outcome.
Step 3 : Clitoris and Clitoral Hood Reconstruction
The clitoris is reconstructed from the dorsal part of the glans penis, using a precise dissection technique to maintain maximum sensory function. Dr. Chettasak meticulously preserves the clitoral neurovascular pedicle, ensuring the branches of the pudendal nerve remain intact to support long-term erogenous sensation.
To provide an aesthetically natural appearance, the clitoral hood is created using a portion of the prepuce skin, mimicking the protective fold of tissue found in natal female anatomy. This step not only enhances the appearance but also helps reduce direct friction on the clitoris, contributing to postoperative comfort and sexual function.
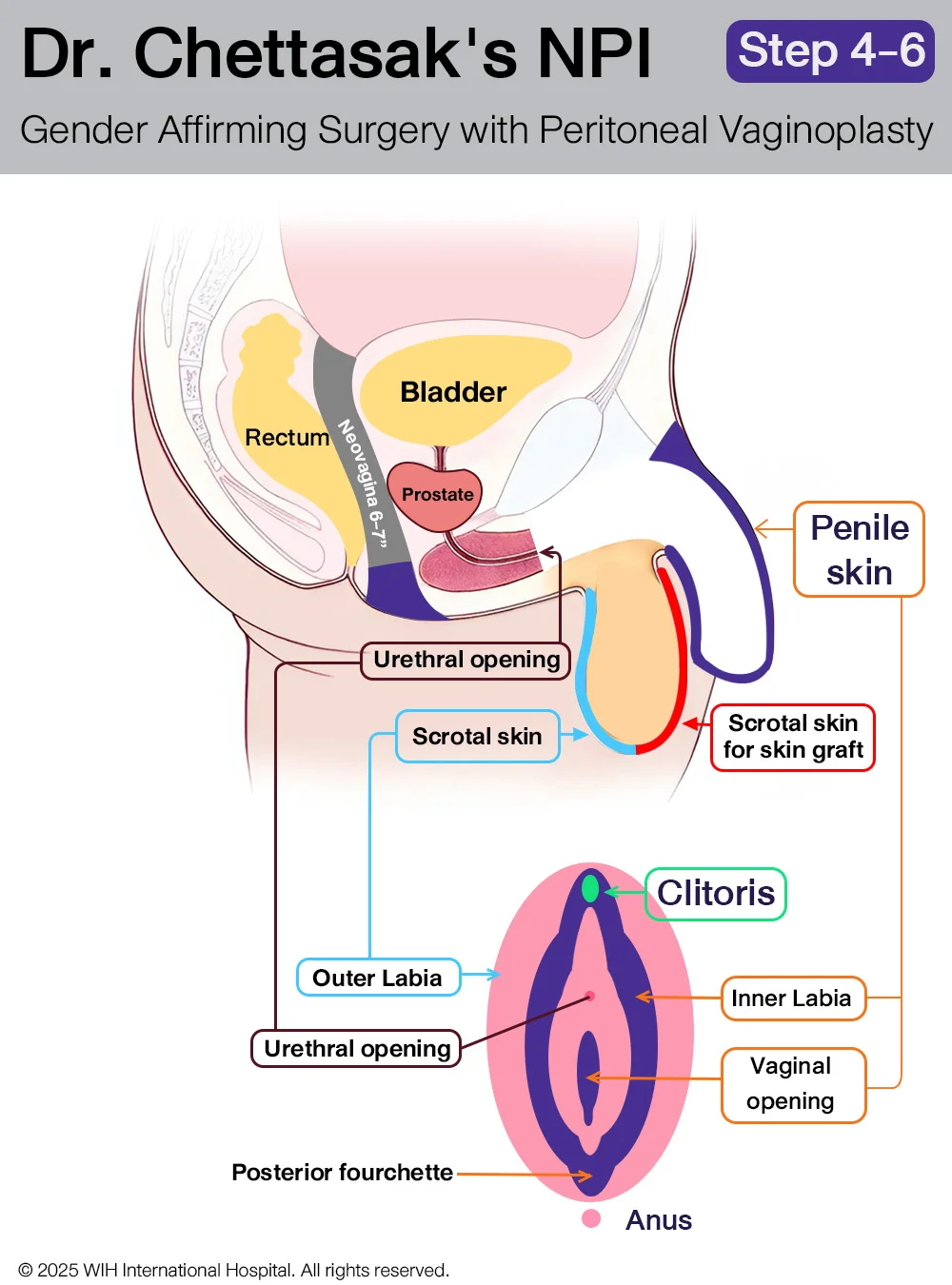
Step 4: Penectomy and Urethral Reconstruction with Penile Skin Preservation
The penis is removed through a careful penectomy, during which the entire corpus spongiosum—the spongy tissue surrounding the urethra—is also completely excised to prevent residual erectile tissue and improve surgical precision.
At the same time, the urethra is shortened and repositioned to align with typical female anatomy. A new urethral opening is reconstructed just above the introitus (vaginal entrance) to mimic the natural female location.
Throughout this step, Dr. Chettasak Tulayaphanich ensures that the penile and prepuce skin are preserved in optimal condition. These tissues will be used in the following step to create the inner labia and a natural-looking vaginal opening as part of Dr. Chettasak’s signature NPI technique.
Step 5: Inner Labia, Vaginal Opening, and Posterior Fourchette Reconstruction
Using the preserved penile and prepuce skin, Dr. Chettasak Tulayaphanich carefully reconstructs the inner labia and sculpts a natural-looking vaginal opening with a delicate V-contour. This approach ensures a feminine and realistic appearance.
A key part of this step is the precise creation of the posterior fourchette—the natural joining point at the lower end of the vaginal opening—using the inner folds of preserved skin. This detail enhances both the aesthetic and anatomical authenticity of the vagina.
This reconstruction method is the signature feature of Dr. Chettasak’s Non-Penile Inversion (NPI) technique, which is globally recognized for delivering superior cosmetic and sensory outcomes in gender-affirming surgery.
Step 6: Outer Labia Reconstruction
The outer labia are reconstructed using the preserved scrotal skin, completing the external genital reconstruction phase.
Surgical Steps for Harvesting the Peritoneal Flap (Laparoscopic Peritoneal Vaginoplasty)
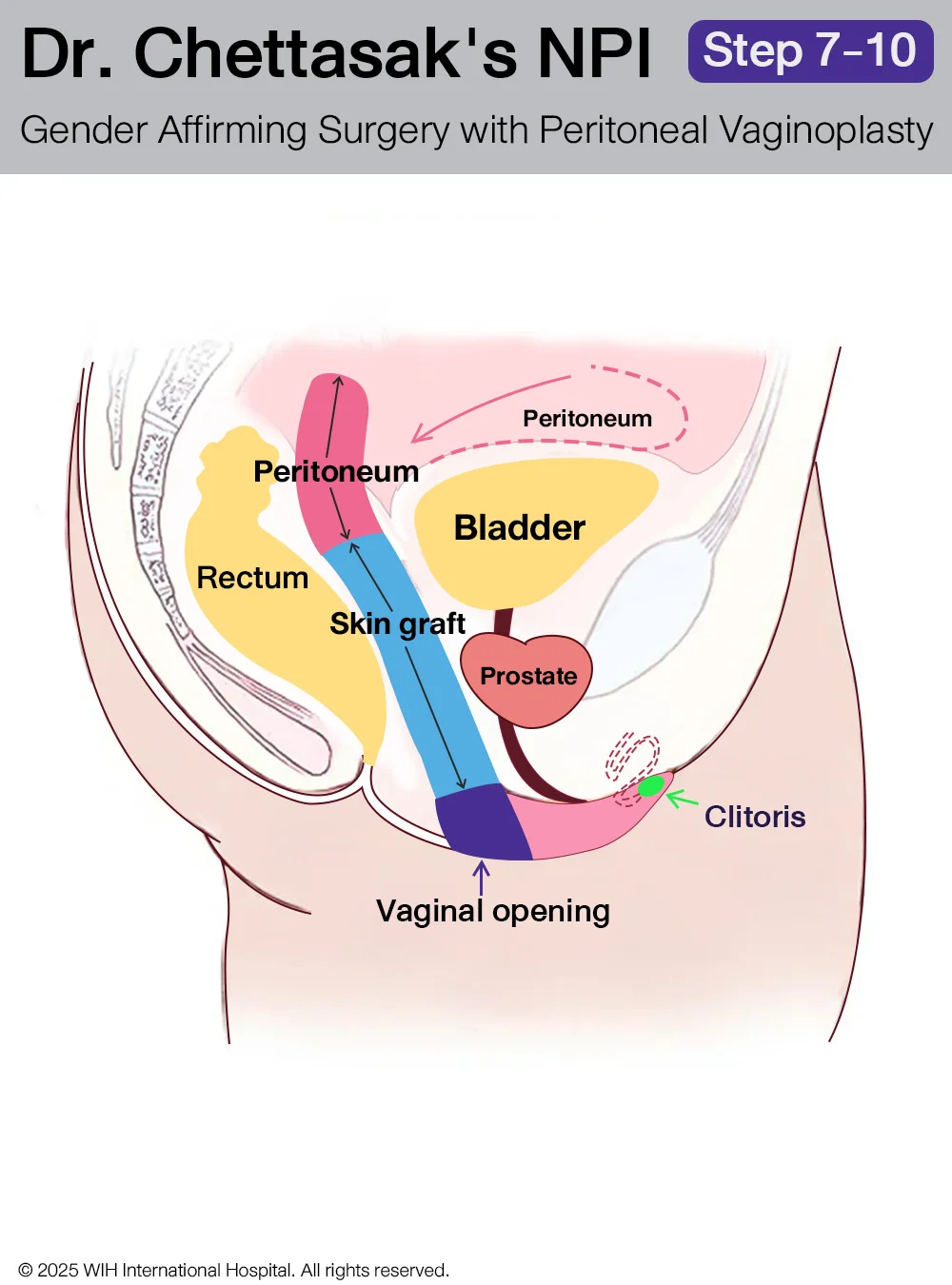
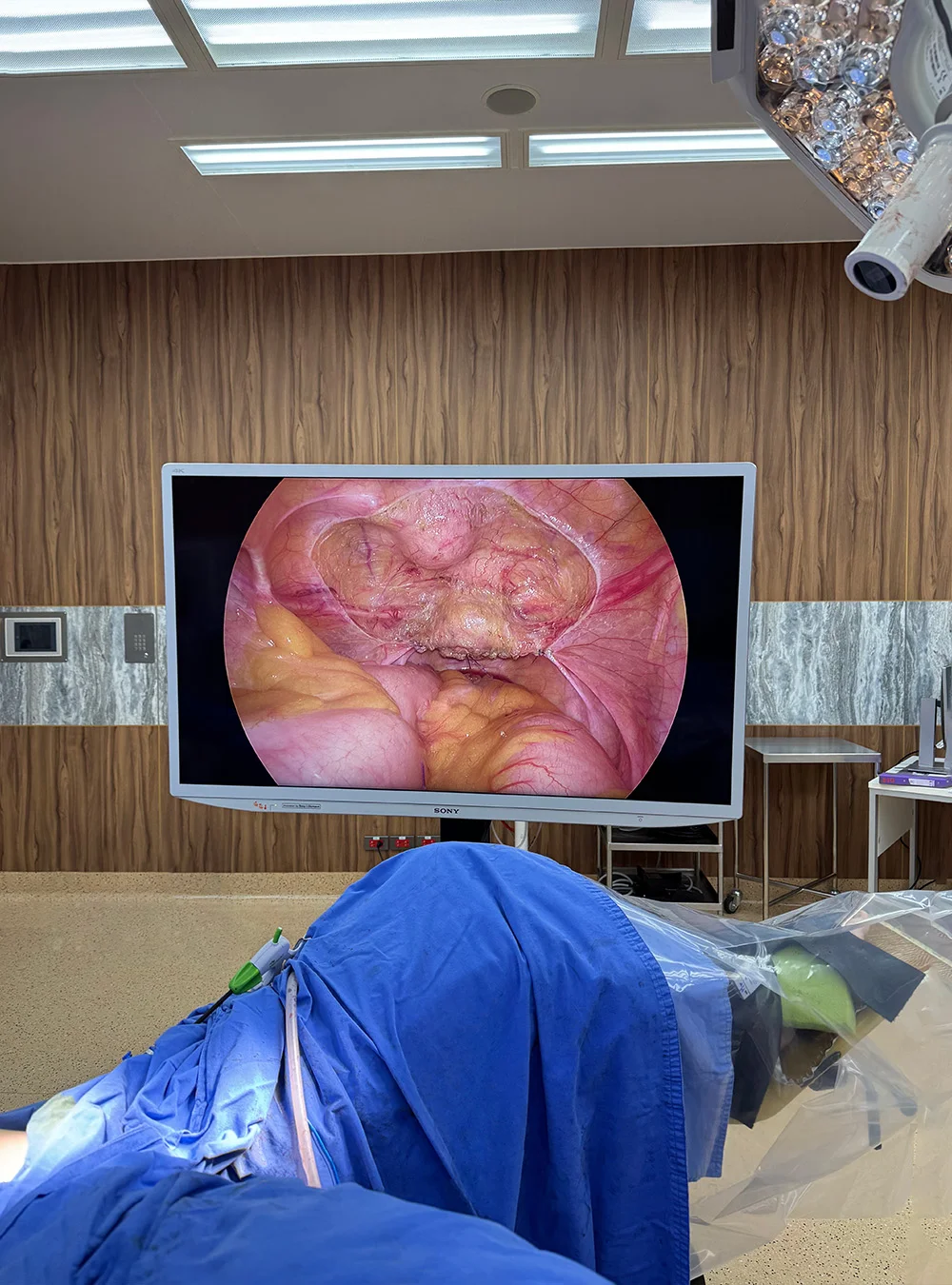
Step 7: Laparoscopic Access & Insufflation
The procedure begins with the insertion of laparoscopic trocars, typically through the umbilicus and lower quadrants. The abdominal cavity is insufflated with CO₂ to create a working space.
Anatomical Exposure
The peritoneal cavity is carefully inspected. The surgical team identifies the vesicouterine space (in patients with Müllerian remnants) or the space between the bladder dome and anterior rectum. The peritoneum overlying the bladder dome, anterior abdominal wall, and lateral pelvic sidewalls is targeted for flap harvesting.
Step 8: Peritoneal Flap Design & Marking
A rectangular peritoneal flap, usually 12–15 cm long and 5–7 cm wide, is outlined on the anterior peritoneum covering the bladder and lower abdominal wall. The flap is designed with a vascularized base to maintain perfusion.
Step 9: Flap Mobilization
Using a combination of sharp dissection and bipolar cautery, the peritoneum is dissected free from underlying structures while preserving small peritoneal vessels. Care is taken not to injure the bladder or inferior epigastric vessels.
Step 10: Proximal Tunneling & Pull-Through Preparation
A vaginal canal tunnel is created through the perineum and into the pelvic cavity. The flap is then gently advanced (pull-through) down into the tunnel and secured to the distal neovaginal margin or to residual mucosa if present.
Anchoring the Flap
The flap is sutured proximally to the pelvic tissues to avoid retraction and distally anchored at the vaginal introitus using absorbable sutures. This forms the proximal neovaginal lining.
A Minimally Invasive Option for Gender-Affirming Vaginoplasty
Peritoneal Pull-Through Vaginoplasty (PPV) is a gender-affirming surgical technique that utilizes peritoneal tissue—a smooth, glistening membrane from the abdominal cavity—to line the innermost portion of the neovagina. This method offers several advantages, especially in terms of texture, appearance, and compatibility with laparoscopic access.
→ What Is Peritoneal Tissue?
The peritoneum is a thin, moist membrane that lines the abdominal and pelvic cavities. When used in neovaginal construction, it provides:
- A smooth, non-keratinized surface that mimics the look of natural vaginal mucosa
- A moist, pink, glistening appearance for aesthetic benefit
- Excellent healing and integration when combined with other graft materials
However, it is important to note that the peritoneum is not a mucosal tissue and lacks secretory glands.
→ Does Peritoneal Tissue Provide Self-Lubrication?
One of the most common misconceptions is that peritoneal tissue provides true self-lubrication. While the peritoneal lining retains surface moisture and appears glistening, it does not secrete fluid like glands found in a biological vagina or in colon vaginoplasty, where natural mucus production is possible.
As a result, patients undergoing peritoneal pull-through vaginoplasty must continue to use water-based lubricating gel during vaginal dilation and penetrative sexual activity, just as those who undergo skin graft techniques. This ensures tissue protection, reduces friction, and supports long-term neovaginal health.
→ How Deep Can the Neovagina Be With PPV?
The final vaginal depth in PPV depends on both patient anatomy and surgical technique. In most cases:
- The peritoneal section provides 4–6 cm (1.5–2.5 inches) of lining at the neovaginal apex
- This is combined with a penoscrotal skin graft to achieve total neovaginal depths of approximately 13–15 cm (5–6 inches)
- The overall depth is comparable to traditional skin graft vaginoplasty and sufficient for most sexual activities
→ Why Laparoscopic Technique Is Required
PPV requires access to the peritoneum inside the abdomen, which must be done through laparoscopic surgery. This minimally invasive technique uses small abdominal incisions and a camera-guided approach for precision harvesting.
Benefits of laparoscopic PPV include:
- Minimal external scarring
- Faster recovery time
- Reduced risk of adhesions or complications
- Precise control over tissue dissection and positioning
→ Is Lubricant Still Required After PPV?
Yes. Despite the moist appearance of the peritoneal lining, it does not produce its own lubrication. All patients must:
- Use water-based lubricants during vaginal dilation and penetrative intercourse
- Avoid dry or high-friction contact that may cause microtears, irritation, or inflammation
- Strictly follow the WIH Hospital vaginal dilation schedule, particularly during the first 1–2 years postoperatively, to maintain depth and prevent neovaginal narrowing

Step 1: Patient Preparation and Positioning
-
Patient placed in lithotomy position
-
Administration of general anesthesia
-
Sterile preparation of surgical field

Step 2: Creation of Vaginal Canal Space
-
Dissection between rectum and urethra/bladder
-
Careful separation to create adequate space for neovagina
-
Hemostasis maintained throughout dissection

Step 3: Peritoneal Harvesting
-
Laparoscopic access to abdominal cavity
-
Identification and mobilization of peritoneal flap
-
Careful preservation of blood supply to peritoneal tissue
Step 4: Peritoneal Pull-Through
-
Transfer of peritoneal flap to vaginal canal space
-
Suturing of peritoneal tissue to create vaginal lining
-
Formation of vaginal apex/cuff
Expert Care at WIH Hospital
At WIH Hospital, Dr. Chettasak and our multidisciplinary surgical team offer advanced laparoscopic-assisted PPV with a focus on safety, aesthetics, and function. Each procedure is customized based on the patient’s anatomy, goals, and tissue availability to ensure optimal long-term outcomes.
Following surgery, patients are required to continue with daily vaginal dilation in accordance with the WIH Hospital Vaginal Dilation Schedule Protocol. Strict adherence to this schedule is essential for maintaining neovaginal depth, preventing tissue contraction, and ensuring the long-term success of the surgery.
→ To learn more or consult about your surgical options, visit the
Gender-Affirming Surgery Center or contact our patient care team.




