General Surgical Complications
These are potential risks associated with any major operation, not specific to GAS:
- Bleeding or Hematoma
Excessive bleeding during or after surgery may require intervention or drainage. - Infection
Although rare, infection can occur in any surgical site and may require antibiotics or further treatment. - Wound Dehiscence
This refers to the surgical wound opening up, which may delay healing and require additional care. - Skin Necrosis or Delayed Healing
Poor blood supply in certain areas may lead to tissue breakdown or the formation of granulation tissue that takes longer to heal. - Scarring or Pigmentation Changes
Most scars heal well, but some patients may develop thickened or darkened scars depending on their skin type and healing response.
Complications Specific to Gender-Affirming Surgery
These issues are more closely related to the techniques used in vaginoplasty or other feminizing procedures:
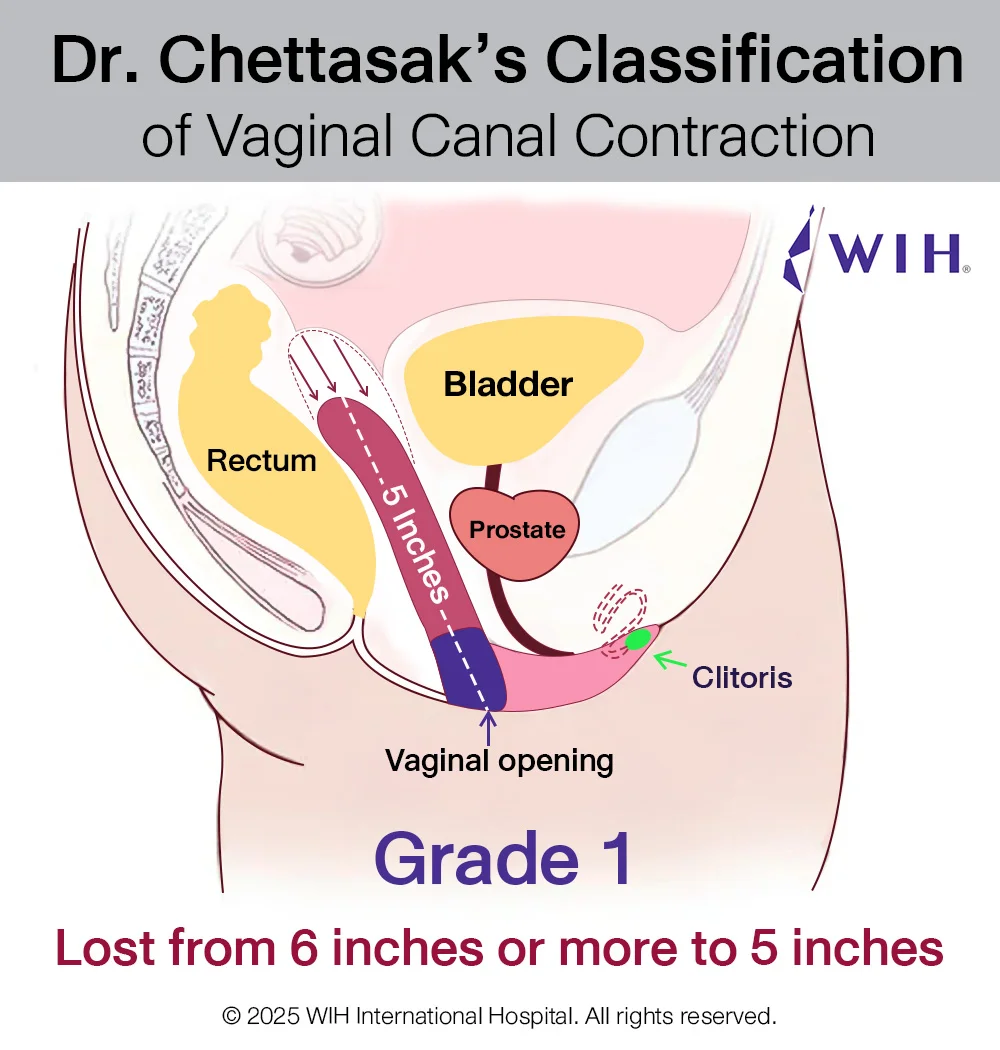
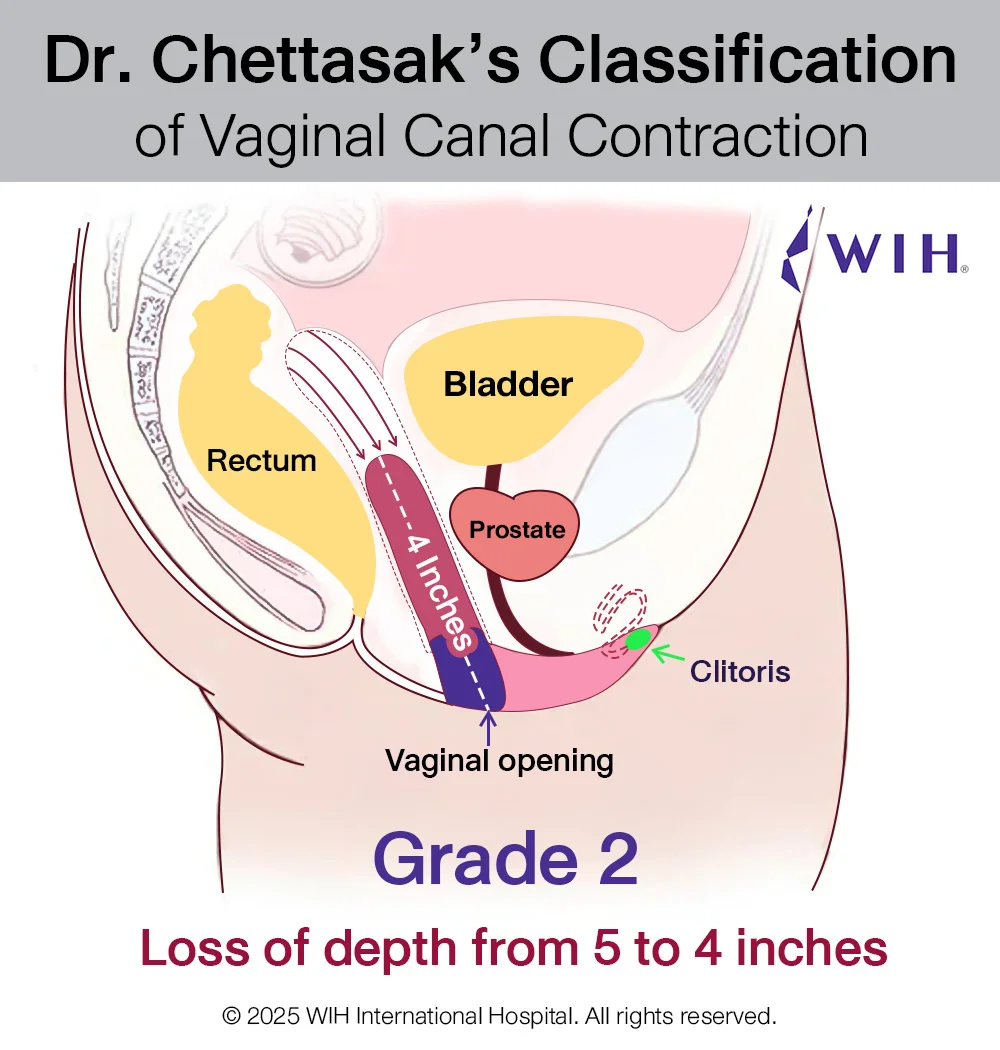
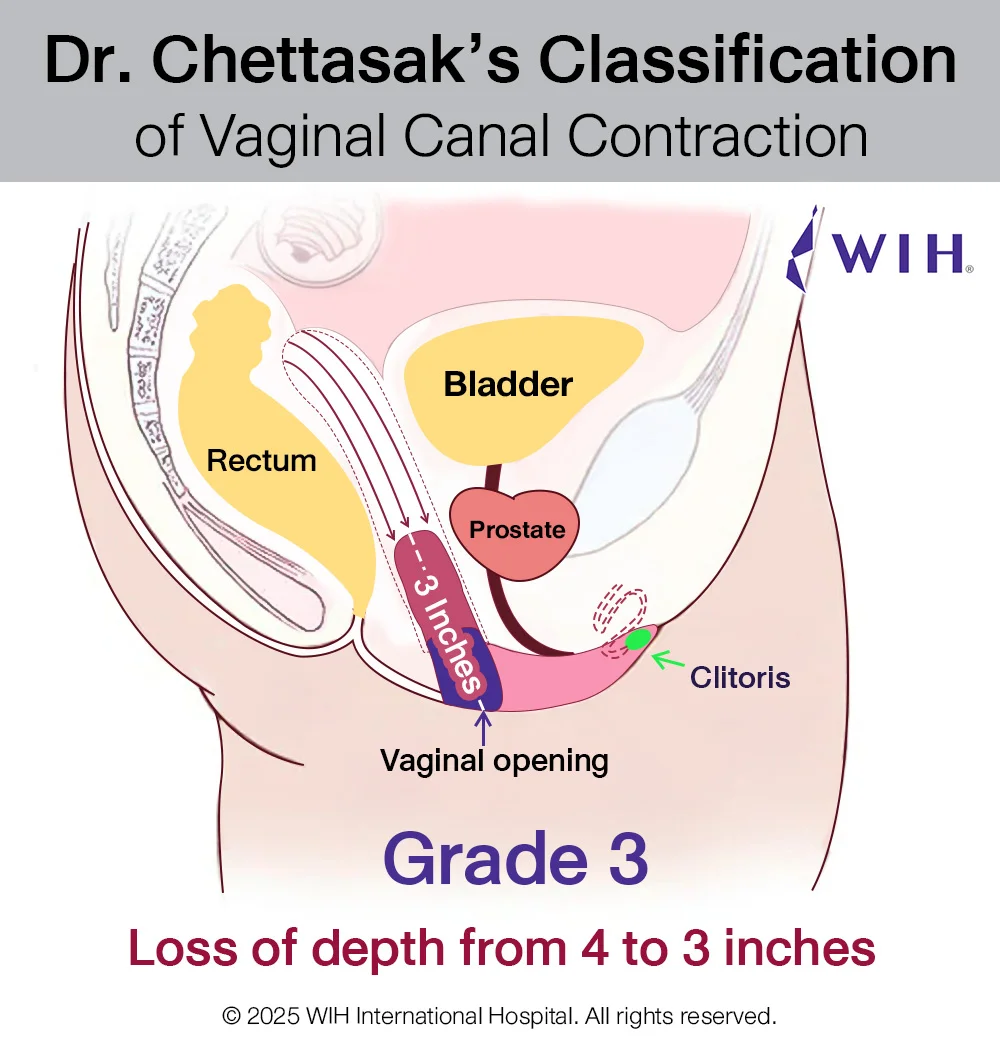
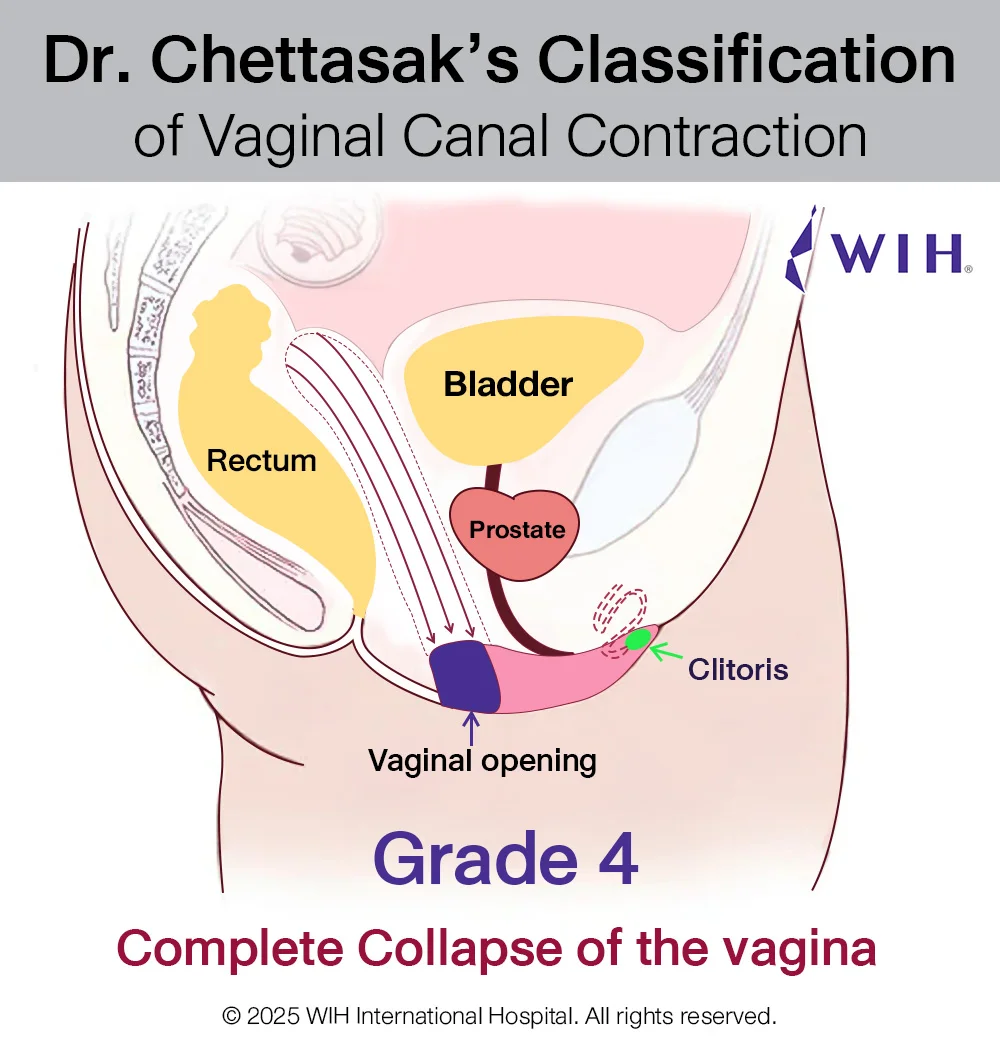
- Vaginal Shortening (Neovaginal Depth Loss)
Common in skin graft vaginoplasty if routine dilation is not maintained or if scar tissue forms at the apex.
Solution: Early intervention, strict dilation regimen, or revision surgery such as colon vaginoplasty. - Vaginal Stenosis or Circumferential Contraction
Progressive narrowing of the neovaginal canal, leading to pain, difficulty with dilation, or inability to engage in penetrative intercourse.
Solution: Depends on severity — from dilation under anesthesia to secondary colon vaginoplasty. - Vaginal Fistula
An abnormal connection between the vagina and nearby organs like the rectum (recto-vaginal fistula) or urethra (urethro-vaginal fistula).
Solution: Multilayered surgical closure, often with reinforcement using well-vascularized tissue such as colon. - Loss of Sensation or Nerve Damage
Although rare with careful technique, sensation in the clitoris or labia may be reduced.
Solution: Often improves over time; nerve-sparing techniques are always used by Dr. Chettasak. - Aesthetic Irregularities
Asymmetry of the labia, irregular scarring, or unnatural appearance may require minor revision for optimal cosmetic outcome.
How WIH Prevents and Manages Complications
Dr. Chettasak Tulayaphanich brings over two decades of experience in gender-affirming surgery with a focus on minimizing risks. At WIH:
- We use precise surgical techniques including the NPI method and laparoscopic colon vaginoplasty.
- We provide a personalized postoperative care plan, including wound care, dilation, and follow-ups.
- Our team offers advanced revision procedures for patients who underwent GAS elsewhere and now face complications.